INTRODUCTION-
Views of scaphoid --> X - rotational (pronation/supination); Y -sagittal (flexion/extension); Z - coronal (radial/ulnar).
• position of immobilization- wrist slightly extended, and the proximal phalanx of the thumb included in a position of slight opposition (“scaphoid cast”).
Views of scaphoid --> X - rotational (pronation/supination); Y -sagittal (flexion/extension); Z - coronal (radial/ulnar).
•The treatment of scaphoid fractures requires knowledge of the blood supply, surgical approaches, and effects that fractures and nonunions of the scaphoid have on carpal kinematics, stability, and arthritis.
• New methods of scaphoid repair have been developed to minimize additional surgical trauma and optimize stabilization until healing.
GENERAL CONSIDERATIONS
INCIDENCE-
• Scaphoid is the “keystone” of the carpus.
•The scaphoid is not only important but it is the most commonly fractured carpal bone. Scaphoid fractures account for 60% to 70% of all carpal fractures and are second in frequency of wrist fractures only to distal radius fractures.
• The majority of injuries are low-energy injuries, either from a sporting event (59%) or from a fall onto an outstretched wrist (35%); the remainder result from high-energy trauma such as a fall from a height or a motor vehicle injury.
• incidence more common in Males than females .
ANATOMY OF THE SCAPHOID
• Skaphos in Greek means Boat, so its a boat shaped bone . Other terms like twisted peanut, as bean shaped are also used to describe this bone.
•Approximately 80% of the scaphoid is covered by cartilage, limiting ligamentous attachment and vascular supply .
• The scaphoid is divided into three regions: proximal pole, waist, and distal pole (tubercle).
•The scaphoid is oriented in the carpus with an intrascaphoid angle averaging 40 ± 3 degrees in the coronal plane and 32 ± 5 degrees in the sagittal plane.
•The scaphoid is the only carpal bone that bridges the proximal and distal carpal rows and acts as a tie-rod.
•carpal rows are supported by stout intrinsic ligaments and reinforced by a volar and dorsal extrinsic ligaments.
• The scapholunate interosseous ligament (SLIL) is a stout ligament connecting the scaphoid to the lunate and is the primary stabilizer. The dorsal region of this ligament resists palmar-dorsal translation and gap due to transverse collagen fibres arrangement, whereas the volar portion resists rotation due to oblique collagen fibers arrangement.
•Radioscaphocapitate (RSC) ligament -
It acts as fulcrum around which scaphoid rotates , scaphoid can also fracture around this fulcrum from Waist .
• Scaphocapitate and Scaphotrapezial ligaments function as primary restraints of the distal pole .
•Vascular Anatomy-
• The blood supply of the scaphoid bone is predominantly retrograde. The major blood supply to the scaphoid is via the radial artery: 70 to 80% of the intraosseous and proximal pole vascular supply is from branches of the radial artery entering distally through the dorsal ridge of the scaphoid between the proximal and distal articular surfaces. The radial artery or the superficial palmar arch also give volar branches that enter in the region of the tubercle and provide the blood supply to 20% to 30% of the bone in the region of the distal pole.
• The proximal pole also gets blood supply from the radioscapholunate ligament (ligament of Testut, a neurovascular conduit) and directs scapholunate branches from the palmar and dorsal transverse carpal arches.
•The more proximal the fracture, the more likely the bone is to be dysvascular and the higher the risk of nonunion. Proximal pole fractures have been reported to have an incidence of avascular necrosis (AVN) of 13% to 50%.
•Combined palmar and dorsal approaches taking off the soft tissue at the tubercle and the dorsal ridge would not be advisable , majority of vessels enter from these landmarks, to be left intact.
BIOMECHANICS OF SCAPHOID FRACTURES
• Hyperextension past 95 degrees is the usual position of injury, but other mechanisms such as axial loading have also been postulated to produce scaphoid fractures.
• Hyperextension mechanism usually causes Volar waist fractures, whereas Proximal scaphoid fractures occur due to dorsal subluxation during forced hyperextension.
• Nonunion occurs in 10% to 15% of all scaphoid fractures.
The risk of nonunion increases with:
1. Delay of treatment for more than 4 weeks
2. Proximal pole fractures
3. Fracture displacement greater than 1 mm
4. Osteonecrosis
5. Tobacco use
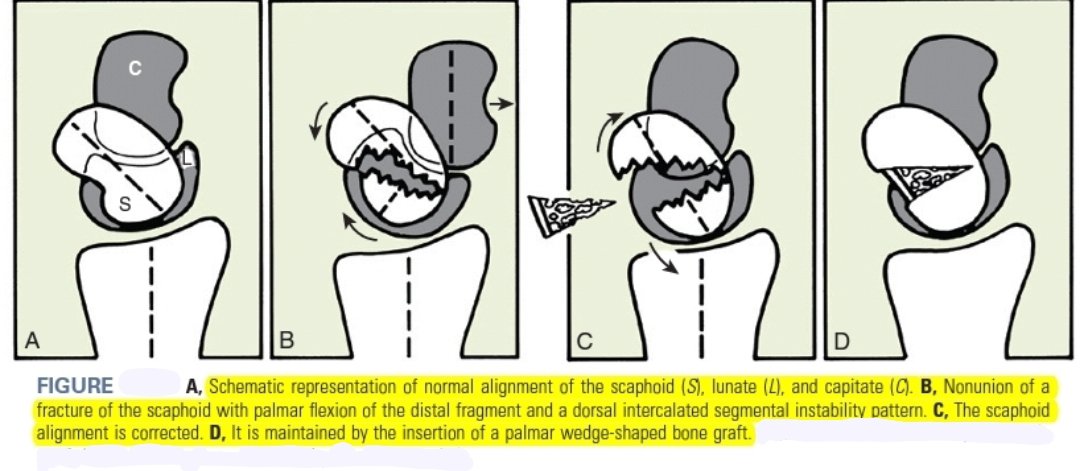
6. Associated carpal instability (DISI = dorsal intercalated segmental instability with a scapholunate angle > 60 degrees and a capitolunate angle > 15 degrees) secondary to humpback (flexed with intrascaphoid angle > 45 degrees; the normal intrascaphoid angle is 24 degrees) scaphoid positioning.
• For nondisplaced waist fractures treated with casting, nonunion rates are 5% to 12%. Nonunion rates for displaced scaphoid fractures treated nonoperatively are higher, reaching 50%.
•Untreated displaced fractures of the waist are subject to varying degrees of these forces and will usually angulate as the volar bone is reabsorbed, yielding a “humpback” of flexion deformity of scaphoid.
• Extension of lunate with its attachment to triquetrum results in a DISI deformity. Ultimate treatment of a humpback scaphoid nonunion with DISI requires both restitution of scaphoid anatomy and reversal of the secondary changes in carpal kinematics.
• Untreated scaphoid nonunion progesses to scaphoid nonunion advance collapse (SNAC) and ultimately Pancarpal Arthritis.
CLINICAL PRESENTATION-
• pain and swelling on the radial side of the wrist .
• history of trauma, such as falling on an outstretched hand, collision of the wrist against a person or heavy obstacle, or possibly a direct blow against an object.
PHYSICAL EXAMINATION-
• On visual INSPECTION , Wrists with acute fractures may have swelling and bruising in the radial aspect.
•“Snuffbox tenderness " which applies predominantly to waist fractures, represent 70% of scaphoid fractures.
•The second most common type of scaphoid fracture is proximal pole fracture, at 20%. The least common is distal pole fracture, at 10%.
PALPATION -
•To palpate the anatomic snuffbox for the waist examination, palpate just distal to the radial styloid in the “soft spot.”
•Distal pole should be palpated at the scaphoid tubercle on the palmar aspect of the wrist just distal to anatomic snuffbox .
•The proximal pole is palpated dorsally in line with the second ray just distal to the dorsal radius lip.
☆ Scaphoid Shift Test / Watson test -
- In normal wrists, the scaphoid cannot flex because of the external pressure by the examiner’s thumb. This may produce pain on the dorsal aspect of the scapholunate (SL) interval owing to synovial irritation.
- A “positive” test is seen in a patient with an SL tear or in a patient with a lax wrist; the scaphoid is no longer constrained proximally and subluxes out of the scaphoid fossa (straight arrow). When pressure on the scaphoid is removed, it goes back into position and typically a clunk occurs.
- Scaphoid shift test has low specificity, in local problems inducing local synovitis (e.g., occult ganglion or dorsal RS impingement), this test may also provoke sharp pain making it difficult to discern whether there is an abnormally subluxable proximal scaphoid.
DIAGNOSTIC IMAGING -
Radiography.
•five radiographic views for the assessment of scaphoid fractures: wrist posteroanterior (PA), lateral, and oblique views; scaphoid view; and clenched pencil view.
•true scaphoid pisiform capitate (SPC) lateral radiograph taken for carpal alignment assessment.
Scaphoid View
Clenched pencil view
Computed Tomography.
•Computed tomography (CT) scanning is helpful to delineate scaphoid fracture displacement, bony morphologic findings, gapping, sclerosis, cysts, and evidence of healing(usually preferred to take at 3 months) . CT is particularly helpful in addressing nonunions. It is important that CT scans are taken with overlapping 1-mm cuts along the long axis of the scaphoid and with coronal and sagittal reconstructions.
•evaluating the vascularity of the proximal pole of the scaphoid.
Magnetic Resonance Imaging.
•Magnetic resonance imaging (MRI) is best to determine whether there is occult scaphoid fracture. Specificity is 90% and sensitivity is between 90% and 100%,as opposed to bone scintigraphy, which is 92% to 95% sensitive and 60% to 95% specific.
•MRI with or without contrast enhancement might be helpful in assessing the vascularity of the bone, but the patient history and CT imaging must be taken into account.
SCAPHOID FRACTURE CLASSIFICATION-
•Scaphoid fractures have been classified by fracture location (proximal, waist, or distal), plane (transverse or oblique), and stability (stable or unstable).
• fracture classification helps in management of injuries,for rapid healing with minimal complications and rapid return to routine activities .
•following classification are used-
1)Russe classification -
The Russe classification predicts instability according to the inclination of the fracture line; for example, vertical oblique fractures.
2)AO classification - The AO classification breaks the fracture down into simple anatomic location (distal pole, waist, proximal pole) and comminution.
3)Herbert and Fisher classification -proposed a classification intended to identify those fractures most applicable for operative fixation and is commonly used throughout the literature .
Herbert and Fisher classified scaphoid fractures according to their stability.
4) Mayo classification-
criteria for instability according to mayo is as follows:
• >1 mm of fracture displacement
• A lateral intrascaphoid angle of >35 degrees
•Bone loss or comminution
•Fracture malalignment
•Proximal pole fractures
•DISI deformity
•Perilunate fracture-dislocation.
NOTE-
* Displaced fracture --> displacement is defined as DISI malalignment of 1 mm [DISI = dorsal intercalated instability with scapholunate angle > 60 degrees and capitolunate angle >15 degrees].
SCAPHOID NONUNION CLASSIFICATION
1) Slade and Geissler Classification
2) Lichtman Classification
3) Alnot Classification
MANAGEMENT OF SCAPHOID FRACTURES -
•Up to 25% of scaphoid fractures are not visible on initial radio-graphs.
•All clinically suspected scaphoid fractures are treated as fractures with short-arm thumb spica cast immobilization until the cause of the symptoms is clarified since failure to treat a stable scaphoid fracture within 4 weeks increases the nonunion rate.
• Follow-up clinical examination and radiograph are taken at 2 weeks .
• MRI is done for diagnosing occult and acute fractures and is generally diagnostic within 24hrs of injury .
SCAPHOID CAST -
• position of immobilization- wrist slightly extended, and the proximal phalanx of the thumb included in a position of slight opposition (“scaphoid cast”).
☆ See here for Scaphoid Surgical Methods .
Mechanics of Fracture Fixation -
• Since majority of the scaphoid is covered with cartilage, fracture callus is not produced, so primary bone healing is entirely dependent on rigid stabilization of the fracture fragments until healing.
•The mechanical effectiveness of internal fixation is determined by the bone quality, fracture geometry, fracture reduction, choice of implant, and implant placement.
•Fracture reduction and placement of the implant in the biomechanically ideal position are the most important of the five variables.
•screws centrally placed in the proximal fragment of the scaphoid had superior results compared with screws placed in an eccentric position.
•Biomechanically, the longer the screw, the more rigid the fixation, because longer screws reduce forces at the fracture site and bending forces are spread along the screws.
• Augmentation with K wires or mini headless screw necessary when central screw placement alone cannot provide rigid fixation.
Techniques for Rigid Fixation
Implants for Rigid Fixation of Scaphoid Fractures -
•Implants used included Kirschner wires, AO compression screws, headless compression screws, plates, and bioabsorbable implants.
SCREWS
☆The difference in pitch between the leading thread (P1) and the trailing thread (P2) of the Herbert screw governs the rate of “take-up,” or drawing together, of the two bone fragments to produce compression.
SURGICAL METHODS-
•Click here for SCAPHOID SURGICAL METHODS
1) Scaphoid Open Reduction and Internal Fixation From the Dorsal Approach/Mini-Open Approach.
2) Scaphoid Mini-Open Screw From the Palmar Approach -
Technical points-
• Place the guidewire as centrally as possible in the scaphoid.
• Consider using an antirotation wire.
• Common error is using a screw that is too long.
• Subtract at least 4 mm from the measured distance.
• A common screw length for an adult male is 20 mm.
• Do not ream past the far cortex .
• If feeling a lot of resistance (especially when reaming over wire), stop and look. The wire may be bent and break or the drill bit may break .
• Beware of hoop stresses. Use countersinking to avoid excessive hoop stresses that can fracture the near fragment.
• Consider the use of joysticks to gain reduction.
• If needed, reduce and pin the lunate in neutral (out of DISI)
• Consider supplemental fixation for more stability.
Delayed presentation of Scaphoid waist fractures -
•Surgery is generally indicated for delayed presentation of a scaphoid fracture 4 to 6 weeks or more following injury.
• patients with delayed presentation have a higher rate of non union .
COMPLEX SCAPHOID FRACTURES
1)Combined fractures of Scaphoid and distal radius -
• Early Surgery is planned in these patients with ORIF of distal radius fracture and mini open approach and fixation for Scaphoid fractures.
2) Transscaphoid Perilunate Fracture-Dislocations
•Perilunate fracture-dislocations represent approximately 5% of wrist fractures and are about twice as common as pure ligamentous dislocations. •Transscaphoid perilunate fracture-dislocation is the most common type of complex carpal dislocation.
• ORIF (via Dorsal approach or Palmar or Proximal row carpectomy ) of these injuries have a good prognosis.
Technical Consideration-
•It is imperative during reduction to restore Gilula’s lines in coronal plane and attain neutral radiolunate and capitolunate alignment in the sagittal plane.
COMPLICATIONS of Scaphoid Fracture Treatment -
•The most common complications are -
1)delayed union,
2) nonunion,
3) arthritis,
4) reduced wrist motion, and
5) loss of strength etc .
MANAGEMENT OF SCAPHOID NONUNION-
☆ Scaphoid Nonunion criteria
failure of union following cast immobilization or surgical treatment of 6 months’ duration.
Evaluation of Scaphoid Nonunion -
•following things to be considered-
1. Site of nonunion , At the waist or at the proximal pole? - more proximal the fracture, the more likely the proximal bone will be dysvascular.
2. Is the nonunion displaced ?
3. Is there a humpback deformity?
4. Is DISI present?
- If there is humpback deformity and carpal malalignment, they may have to be corrected at the time of bone grafting and fixation.
5. Is there comminution, cyst formation, or cavitation?
• If the nonunion is stable and well aligned and bone loss is minimal, limited opening in the nonunion site, curetting as necessary, and cancellous bone grafting may be appropriate, followed by internal fixation by a headless compression screw.
6. Was there previous surgery?
-Any previous surgical or other treatments should be taken into account because they would make further treatment more complex.
7. Does the proximal pole look dysvascular?
-In cases of diminished vascularity bone grafting have to be considered.
- According to Green, vascularity was best determined by punctate bleeding. MRI also helpful .
8. Is there arthritis (SNAC wrist)? If so, at what stage?
- if early arthritis (SNAC I) is confined to the radial styloid, radial styloidectomy and scaphoid bone grafting could be considered.
- In advanced arthritis with mild symptoms, nonoperative management is considered .
- In arthritis with severe symptoms , other options may include partial denervation or salvage procedures such as scaphoid excision and four-bone fusion, proximal row carpectomy, total wrist fusion, hemiwrist arthroplasty, and total wrist arthroplasty.
9. Is the scaphoid deformed or salvageable?
- sometimes the proximal or distal pole has fragmented and is not usable .
Treatment algorithm-
HYBRID RUSSE PROCEDURE-
The hybrid Russe procedure is advantageous because it is effective for humpback scaphoid nonunions with DISI.
Steps -
• Exposure of nonunion site
• uptake of bone graft
• Packing of Graft into the Nonunion site
• Internal fixation with headless screw
VASCULARIZED BONE GRAFTING
Common choices are -
1. 1,2 intercompartmental supraretinacular artery (ICSRA) pedicle (Zaidemberg)
2. Pedicled on the volar carpal artery (Mathoulin)
3. Dorsal capsular pedicle (Sotereanos)
4. Free medial femoral condyle graft (Doi, Bishop and Shin, Higgins
Surgical Fixation of Scaphoid Nonunion With Nonvascularized Bone Graft (Distant) Wedge Graft
Fernandez-Fisk wedge graft. -
• This procedure is use to treat scaphoid nonunion with carpal instability.
STEPS -
(1)preoperative calculation of the exact scaphoid length and form based on comparative radiographs of the opposite wrist, (2) the use of a palmar approach, (3) the insertion of a wedge-shaped corticocancellous graft from the iliac crest after resection of the pseudarthrosis, and (4) the use of internal fixation.
Anterior Wedge Grafting -
Unsalvageable Scaphoid Proximal Pole Nonunion -
Rib osteochondral autograft reconstruction of the proximal pole.
Salvage Procedures for Scaphoid Nonunion Advanced Collapse
1) Radial Styloidectomy . - good for stage I SNAC arthritis when combined with procedures to heal scaphoid nonunions.
2) Distal Scaphoid Resection Arthroplasty.
•Indicated in waist fracture nonunion with SNAC I styloscaphoid arthritis with significant loss of wrist dorsiflexion and radial deviation and pain on wrist loading, gripping, and range of motion.
3) Proximal Row Carpectomy .
• it is a simple motion preserving salvage operation done ideally in a relatively low-demand patient older than 40 years with stage II or III SNAC with no to minimal capitolunate degenerative disease.
• removal of proximal row starts with Scaphoid then Lunate and then Triquetrum with taking care not to damage the articular surface of the head of the capitate.
• Avoid injury to RSC ligament that prevents postoperative Ulnar translocation of the carpus.
4) Intercarpal Fusion.- Fourbone (capitate-lunate-hamate-triquetrum) fusion with scaphoid excision satisfactorily treats degenerative SNAC arthritis affecting the radioscaphoid and midcarpal joints while preserving an anatomically congruous radiolunate joint.





































It's really amazing information thank you
ReplyDeleteMini Fragments Implants & Instruments
Mini Fragments Locking Compression Implants & Instruments
Small Fragments Implants & Instruments
Small Fragments Locking Compression Implants & Instruments
Large Fragment Implants and Instruments
Large Fragment Locking Compression Implants & Instruments
DHS/DCS Implants & Instruments
Angle Blade Plate Implants & Instruments
Thanks for sharing such amazing content.
ReplyDeleteSee The Best Wrist Surgeon Specialist - Dr. Philip Mathew
Your blog is wonderful I like reading your articles Always. Stay up with the great work! You realize, lots of persons are looking around this info, you could aid them greatly work.
ReplyDeleteBest Orthopaedic Surgeon in Shastri Nagar
Orthopaedic Surgeon in Shastri Nagar
Best Dentist in Shastri Nagar