Introduction
Epidemiology
Risk factors
Injury Mechanism
NORMAL RADIOLOGICAL PARAMETERS OF DISTAL RADIUS AND ULNA -
Parameters to check in Distal radius #
CLASSIFICATION-
2) Displaced distal radius fracture-
Type of Cast. The initial cast is usually a Below elbow Slab or Sugar tong splint. These allow for swelling to occur in the cast.
REDUCTION MANEUVER
The recommended position of immobilization for a dorsally angulated metaphyseal fracture is neutral to slight flexion, 20 to 30 degrees of ulnar deviation with neutral forearm rotation. Radiographs are obtained to confirm reduction. Although palmarly displaced, extraarticular Smith fractures are generally unstable, the flexion–pronation deformity of them can be reduced and occasionally stabilized effectively in extension and supination (45-60 degrees) with a sugar tong splint.
• Percutaneous fixation and bridge plating, should be considered alternative to Open anatomic reconstruction in cases of extreme articular comminution . In these type of cases, efforts should be focusing at restoring the anatomic relationships of the radius and ulna and to ensuring normal alignment of the hand and carpus with the long axis of the forearm by percutaneous and indirect means.
3)MANAGEMENT OF UNSTABLE EXTRA- ARTICULAR/MINIMAL ARTICULAR DISTAL RADIUS FRACTURE-
- Distal radius Fractures are one of the most common Fractures encountered by Orthopedic Surgeon worldwide.
- PETIT 1st said these injuries as Fractures rather dislocation.
- POUTEAU recognized injuries to the wrist from fall onto outstretched hand.
- ABRAHAM COLLES described these Fractures one and half inch above the carpal extremity of the radius.
- MALGAIGNE in 1847 stated these injuries caused due to fall on the palm of hand. He identified extra- and intra- articular fractures.
- JOHN RHEA BARTON described subluxation of the wrist after fracture through distal articular surface of radius.
- Robert Smith described fracture of distal radius with lower fragment displaced forward.
Epidemiology
- Females > males ( 2:1 )
- AGE - in females = common in their 6th decade males = common in their 4th decade
- Low energy injuries ( 70%) > high energy injuries (10%)
- Majority of Fractures ( ~ 60%) are extra articular (AO type A), 10% are partial articular (AO type B), 30% are completely articular (AO type C)
Risk factors
- Low BMD (Bone mineral density).
- Increasing falls especially with aging is a significant risk factor.
Injury Mechanism
- Fall onto outstretched hand from standing height mainly , small proportion of patients have high velocity injury.
- Distal radius # resulted if angle at which forearm strike the ground was between 60 and 90 degrees with ulnar deviation resulting in radial styloid # and radial deviation results in ulnar styloid # .
- Frykman concluded clinical types of distal radius # occur when dorsiflexion of the wrist was between 40 and 90 degrees. If more then a carpal bone # and if less a proximal forearm # resulted .
- Fernandez divided distal radius Fractures based on the mechanism of injury.
Associated Injuries with Distal radius and Ulna Fractures
- TFCC ( Triangular FibroCartilage Complex ) INJURY- more common than interosseous ligament injury, reported in 39% to 82% of cases.
- Majority are peripheral avulsions and may be associated with ulnar styloid # , the presence of which increases the risk of TFCC tear by a factor of ~ 5.
2. INTEROSSEOUS LIGAMENT INJURY- predominantly Scapholunate and Lunatotriquetral injury.
- Geissler graded these injuries Arthroscopically , Grade 1 being least severe with only attenuation or hemorrhage and Grade 4 is gross instability with sufficient disruption.
- Diagnosis of ligament injury can be done with Static radiographs of the distal radius in the more severe cases but diagnosis can be difficult with a distal radius # .
- Arthroscopy is probably the best method , another method is Carpal stretch test in which traction is applied to the wrist to emphasize disruption of Gilula's lines.
- There is increased risk of interosseous ligament injury , been demonstrated when there is more than 2 mm of positive ulnar variance and in intra-articular fractures.
SIGNS AND SYMPTOMS
- Pain and swelling around the wrist .
- Visible Deformity in cases of displacement.
- Any paresthesia or numbness in the fingers to rule out any median or ulnar nerve injury.
- Pain elsewhere in the limb suggest ipsilateral injury.
- The classical dinner fork or silver fork deformity is due to dorsal displacement of the carpus secondary to dorsal angulation of the distal radius.
- The reverse deformity is seen in volar displaced fractures.
- The hand may be radially deviated and if shortening of the radius the ulna will be prominent.
- Skin inspection to rule out any open wounds, common on ulnar side.
- Palpation of the fracture will elicit tenderness.
- Thorough neurological testing of the hand should be done as acute carpal tunnel syndrome (CTS) may require prompt treatment.
NORMAL RADIOLOGICAL PARAMETERS OF DISTAL RADIUS AND ULNA -
Parameters to check in Distal radius #
- Radial length
- Radial inclination
- Ulnar variance
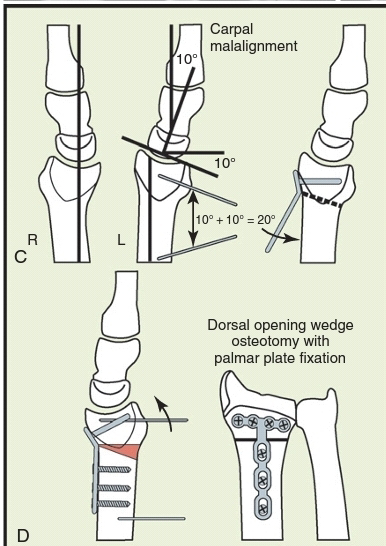
- Carpal malalignment

Carpal malalignment - Tear drop angle
- A-P distance
CLASSIFICATION-
A- Extraarticular
B- Partial Articular
1) Undisplaced distal radius fracture-
2) Displaced distal radius fracture-
REDUCTION MANEUVER
The recommended position of immobilization for a dorsally angulated metaphyseal fracture is neutral to slight flexion, 20 to 30 degrees of ulnar deviation with neutral forearm rotation. Radiographs are obtained to confirm reduction. Although palmarly displaced, extraarticular Smith fractures are generally unstable, the flexion–pronation deformity of them can be reduced and occasionally stabilized effectively in extension and supination (45-60 degrees) with a sugar tong splint.
The three-point bending principle should be used to help maintain reduction; first dorsal molds are applied over the metacarpals and the second over mid-diaphysis of the radius, and a third palmar countermold is placed over the apex of the fracture. “Six-pack” digital exercises are begun immediately to reduce edema and prevent contractures and disuse atrophy.
PERCUTANEOUS PIN FIXATION -
Percutaneous pinning, supplemented by an external fiberglass cast, is a relatively simple and effective fixation method that is applicable for reducible extraarticular fractures and simple articular fractures without metaphyseal comminution but with good bone quality.
Care must be taken to avoid injury to the dorsal sensory nerves, particularly when transfixing the radial styloid.
KAPANDJI TECHNIQUE
Kapandji popularized the technique of “double intrafocal wire fixation” to both reduce and maintain distal radial fractures. This technique is best reserved for simple extraarticular fractures and is not without complications.
EXTERNAL FIXATION-
1)Bridging or spanning fixation and
2)Non-bridging or non-spanning fixation
AUGMENTED EXTERNAL FIXATION(Bridging)-
Indications
• Unstable extraarticular fractures of the distal radius (type I bending)
• Impacted articular fractures (type III compression)
• Comminuted unstable fractures with articular and metaphyseal involvement
Contraindications
• Severe osteoporosis
• Volar shear fractures (type II; Smith type II; volar Barton type)
• Patient preference, compliance concerns, or inability to care for the external fixation and pins
Technical points -
• Closure of pin cluster incisions before assembly of the fixator
• Gross alignment of the fragments by fixation in moderate traction, flexion, and ulnar deviation
• Assessment of the DRUJ for stability and augmentation as needed
• Apply a sugar tong splint in supination for 5 to 10 days until suture removal.
• Start digital range-of-motion exercises immediately.
Non-bridging or non-spanning external fixation
Indications -
•fractures of the distal radius with actual or predicted instability, which are extra-articular or have an articular extension, which is undisplaced or reducible closed. There must be sufficient space in the distal fragment to site the pins. This usually requires 1 cm of intact volar cortex.
Arthroscopic Reduction and Percutaneous Fixation Technique-
•If considering arthroscopically assisted reduction and fixation of an articular distal radius fracture, it is good to reduce and stabilize the fracture in a splint for 3 to 7 days before planning surgery. Treatment of fractures acutely by arthroscopic means may limit visibility due to bleeding and may risk the development of compartment syndrome because of extravasation of fluid into the soft tissues. After 7 days, however, it becomes difficult to elevate impacted articular fragments without a formal open reduction.
Bone Graft and Substitutes -
• Supplemental bone graft is now most often used in subacute or nascent malunions requiring osteoclasis ; malunited fractures; and, less frequently, in the acute situation to buttress the reduction of small articular fragments
• The use of a bone graft has dramatically decreased during the last 5 years to supplement internal or external fixation.
Open Reduction and Internal Fixation(ORIF)-
Indication-
• In active patients where satisfactory reduction cannot be maintained/achieved by closed manipulation and casting,
• As an alternative to percutaneous fixation because of preference of patient or surgeon.
CONTRAINDICATIONS-
•Articular fractures of elderly, inactive patients, and in those with considerable osteoporosis.
VOLAR OR DORSAL APPROACH -
The surgical approach to be preferred depends mainly on the location and direction of displacement of the fracture fragments. Therefore, dorsally or radially displaced fractures have been classically approached through dorsal incisions, whereas volarly displaced fractures (e.g., the Smith and reversed Barton) are classically approached through palmar exposures.
VOLAR PLATING-
Advantages of palmar exposure and volar plating :
• Minimal volar comminution facilitates reduction of dorsally displaced fractures.
• Anatomic reduction of the volar cortex facilitates restoration of radial length, inclination, and volar tilt.
• Preservation of the vascular supply of comminuted dorsal fragments due to avoidance of additional dorsal dissection.
• Since the wrist’s volar compartment is having larger crosssectional space and the implant is separated from the flexor tendons by the pronator quadratus, the flexor tendon complications incidence is minimized.
• Use of fixed angle volar plate avoids “toggling” of screw in the distal fragment and thus reduces the danger of secondary displacement.
• With help of a fixed-angle, internal-fixation device that uses subchondral pegs or screws, shortening and displacement(late) of articular fragments can be controlled and that reduces the need for bone grafting.
Exposure-
•Through the distal part of the Henry approach in between the FCR and radial artery via an 8- to 9-cm longitudinal incision.
• "Hockey-stick” extension can be made toward the scaphoid tubercle if additional exposure is required.
• Detach the pronator quadratus with an “L”-shaped incision and leave a portion of the split BR attached to the pronator for subsequent closure.
Technical Considerations-
•Avoid placement of plate distal to the transverse radial ridge (i.e., the so-called “watershed” line) because implants on the volar lip of the radius are in direct continuity with the flexor tendons, and there is a risk of tendon irritation and rupture. Hardware placed 2 mm or more above the volar critical line (Soong Grade 1) or within 3 mm of the distal edge of the volar rim (Soong Grade 2) has been demonstrated to have a high rate of tendon rupture.
• For Irreducible Articular fractures(to visualize the dorsal die-punch and centrally impacted fragments) , an extended FCR approach is an option:
a) Perform a tenotomy of the BR tendon.
b) Release the first dorsal compartment.
c) Pronate the proximal fragment to expose the articular surface.
FRAGMENT SPECIFIC FIXATION-
Robert Medoff devised a hybrid technique of percutaneous wire and plate fixation designed to fix individual fracture fragments through several small incisions. His “fragment-specific” classification defines articular fractures of the radius by recognition of five elemental fragments present alone or in combination in every fracture. Implants are placed strategically along the radial and intermediate columns to maximize construct rigidity.
Mechanical studies using an unstable metaphyseal fracture model have proved superiority of dual 2.0 mm plates placed at 50- 90 degrees to each other in axial plane compared to that of either K-wire–augmented external fixation or to a traditional 3.5-mm dorsal “T”-plate.Thus, the use of the term “fragment-specific fixation” does not refer to a particular implant type but to the concept of the use of two or more low-profile implants placed strategically along the columns of the distal radius to fix individual fracture fragments.
Examples-
1) Comminuted Dorsal Cortex
2) Dorsal Intermediate Column Fragments
3) Volar Ulnar Corner
INTRA-MEDULLARY IMPLANTS -
Novel intramedullary (IM) methods have now been developed for rapid restoration of radial length, alignment, and tilt; they are designated lowprofile, minimal-incision alternatives to other previous methods.
3)MANAGEMENT OF UNSTABLE EXTRA- ARTICULAR/MINIMAL ARTICULAR DISTAL RADIUS FRACTURE-
(1) early mobilization,
(2) closed treatment and cast immobilization with or without radioulnar pinning, and
(3) operative management, including open and arthroscopic techniques.
Assessment-
assess radioulnar stability after completion of radial fixation, a manual “shuck” test of the ulna is performed by grasping the ulnar head between the examiner’s thumb and index finger and translating it dorsally and palmarly within the sigmoid notch. Gross instability is manifested by frank dislocation, but more subtle instability can be appreciated by the loss of a firm endpoint to translation and by increased subluxation of the ulna relative to the uninjured wrist.
COMPLICATIONS-
1) NERVE INJURY-
•MEDIAN NERVE INJURY is the most common nerve associated with distal radius fracture which presents as Carpal Tunnel Syndrome (CTS).
• presents in between 3% and 17% of fractures.
Causes -
contributory causes of early CTS after distal radius fracture are swelling and hematoma extending into the carpal canal or deep to the fascia at the level of the fracture, direct nerve contusion, hematoma block,and the Cotton-Loder position.
CTS can present at different intervals :
1. Acute—within 1 week of fracture (27.4%).
2. Subacute—1 to 12 weeks after fracture (44.3%).
3. Delayed—more than 12 weeks after fracture (28.3%)
The acute onset group was younger and contained significantly more males, high-energy injuries, and AO type C injuries . While other two groups were having lower energy injuries and older womens .
• Decompression is successful in the majority of patients,but sometimes compression may occur proximal to the wrist crease at the level of the fracture and release should be extended to this area.
ULNAR NERVE INJURY is less common than median nerve injury
• risk factors are instability of the DRUJ open fractures, high-energy injury, and severe fracture displacement.
•Most of these injuries are neurapraxias which recover spontaneously. Exploration is recommended where there is complete ulnar palsy with an open wound or concurrent acute CTS.
2)TENDON INJURY-
•Most commonly EPL Tendon(Extensor Pollicis Longus )
• Can be due to Hardware related or fracture related causes.
•Hardware-related ruptures most commonly occur with volar or dorsal plating and are discussed previously in the relevant sections.
• fracture-related ruptures occur earlier after injury at an average of around 6 weeks whilst later ruptures may be more likely to be related to attritional problems on hardware.
•Fracture-related flexor tendon injuries are much rarer possibly because the muscle belly of pronator quadratus acts as a cushioning layer between the flexor tendons and bone.
• If functional problem occurs after EPL rupture then tendon transfer, usually with extensor indicis proprius, should be considered.
3) MALUNION -
•Malunion of distal radius fracture is common , although it is not frequently reported.
•Typical symptoms of malunion are as follows.
1. Pain
—ulnar sided
—carpal
—radiocarpal
2. Weakness of grip
3. Reduced range of movement, especially rotation
4. Deformity
•Pain is a common symptom of distal radius malunion and can be located in the DRUJ, the carpal area or the radiocarpal joint .
•Treatment of Symptomatic Malunion In the fit independent patient is surgical(distal radial osteotomy ).
4) NONUNION-
•Nonunion of the distal radius is rare occurring in well under 1% of fractures and may occur in the presence of extensive metaphyseal comminution. The diagnosis is made in the presence of continuing pain and increasing deformity. It is usually treated with plating and bone grafting to which most nonunions are amenable even with small distal fragments.Wrist fusion should be reserved for cases where plating and bone grafting fail.
5)Complex Regional Pain Syndrome (CRPS)-
CRPS is a serious and often debilitating complication of a number of injuries but is most commonly seen after distal radius fracture. Its etiology is unknown and it is characterized by a number of symptoms and signs including pain, swelling, color and temperature change, and joint contracture.
















































No comments:
Post a Comment