INTRODUCTION
* At least 7% of all tibial plateau fractures lie in the region of the posterolateral corner. Fractures in this region, usually cannot be adequately treated by using a lateral or anterolateral approach due to coverage by the fibular head and ligamentous structures in the corner region of the popliteus muscle.
• To minimize this problem, a lateral approach was described by Lobenhoffer et al.With this approach, a fibular osteotomy and detachment of the joint capsule and meniscotibial ligaments from the lateral tibial plateau allow for the exposure and examination of the posterolateral joint surfaces of tibia.
• Lobenhoffer approach provides a good view of the posterolateral corner of the tibial plateau but leads to extensive trauma of soft tissue there.
• Isolated posterior approaches allow for fragment fixation but visual control of fracture reduction is limited.
* Therefore a modified surgical technique for the treatment of posterolateral tibial plateau fracture was introduced. Frosch described this posterolateral approach for fracture reduction and fixation combined with a lateral arthrotomy to visually control the fracture alignment and the joint surface.
SURGICAL TECHNIQUE-
POSITION-
• Patient lies in a lateral position.
• Knee is supported by thick rolled pillow because the weight of the leg itself apply varus stress which causes the joint gap to be laterally opened.
INCISION-
• An approximately 15 cm long posterolateral skin incision is required. Fibula head is used as an anatomical landmark.
•Incision starts 3 cm above the joint line and follows the fibula in a distal direction.
•Before the popliteal fossa is dissected a lateral standard arthrotomy is performed.
EXPOSURE-
•The iliotibial tract is incised from the dorsal side and the dorsal fibers are detached from the Gerdy's tubercle. Thereafter, the lateral capsule is incised and the meniscotibial ligament is dissected approximately 2mm away from its insertion in the tibia, parallel to the joint surface.
•The entire lateral tibial plateau, including the posterolateral corner can be viewed by using this lateral arthrotomy.
•For manipulation of the posterolateral fragment an additional posterolateral exposure of the fragments is necessary.
• Both approaches are performed through one skin incision.
• After direct incision of the fascia, the peroneal nerve is exposed to the rear edge of the biceps femoris muscle. The nerve should be carefully dissected and gently mobilized for protection during the operation.
• Blunt dissection of the popliteal fossa is initially performed between the lateral head of gastrocnemius and soleus and inspection begins on the muscle belly of soleus.
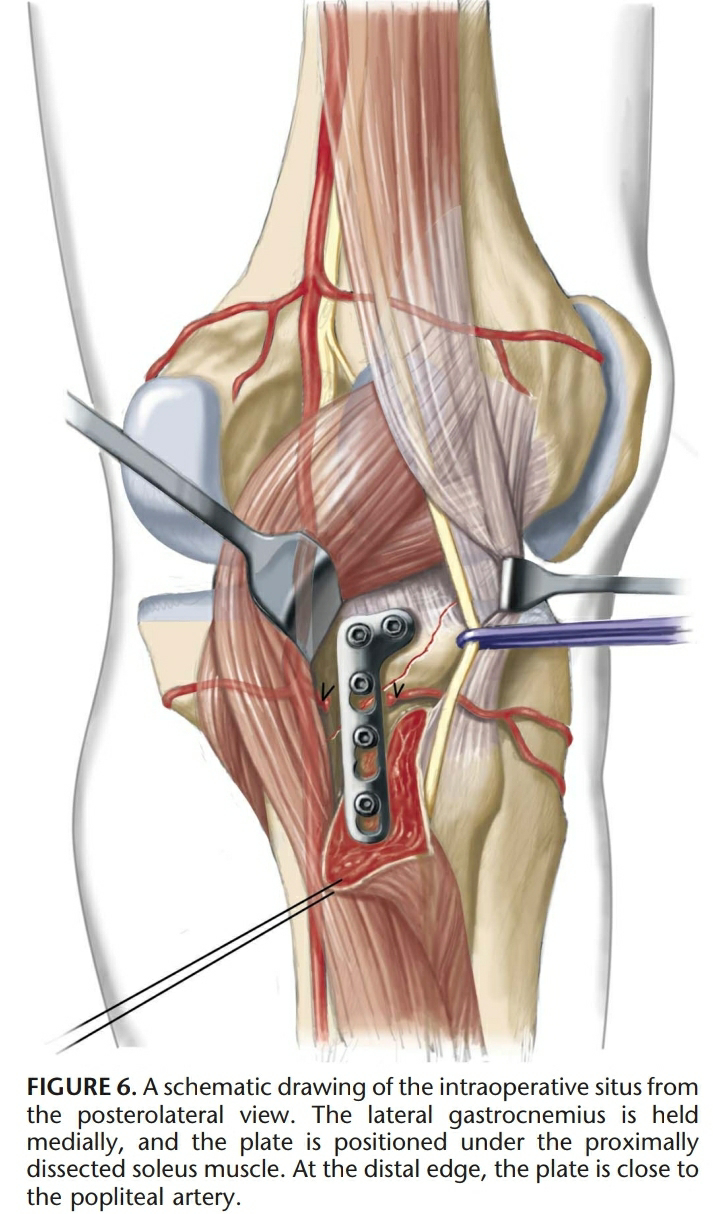
• Popliteal vessels and the popliteus muscle are exposed.The popliteal vessels are protected by the lateral head of gastrocnemius which is retracted by a Langenbeck retractor.
•Inferior genicular vessels are ligated only if necessary.
•At distal edge of the popliteal muscle, it is pulled back towards the medial and cranial direction. Then the muscle is carefully detached from the dorsal surface of the fibula.
•The soleus muscle should be detached distally until the peroneal nerve at the fibular neck enters into the musculature. The peroneal nerve should not be detached after it enters into the musculature because muscle branches leading off in a atypical fashion can be easily damaged.
FIXATION-
•Posterolateral fragments are manipulated and reduced from the dorsal side with a raspatory or with pointed reduction forceps.
•Fragments after reduction are held in place using K wires.
•Plain radiographs need to be performed intraoperatively.
*After fracture reduction, a conventional radius, T plate can be pinched off with lateral gutters so that a two-hole L-plate is obtained. To buttress the fracture, the plate can be slightly under countered and dorsally fixed with conventional screws.
The lateral edge of the plate lies immediately next to the fibular Head.
ADVANTAGES-
1) Visual control of the reduction of the fracture is achieved through a conventional lateral standard arthrotomy, which is accomplished through the same skin incision. The anatomical reduction of the fracture and internal fixation are performed from the dorsal side. Therefore as a result of the modified posterolateral approach, the fragments are not denuded.
2) The avoidance of fibula osteotomy in most patients with posterolateral tibial plateau fractures is an advantage.
3) Damage to the upper tibiofibular joint and nerve injuries caused by an oscillating saw blade can be avoided by using the presented technique.
4) Minimal soft tissue damage compared to Lobenhoffer posterolateral approach with fibular osteotomy.
Limitation of the modified posterolateral approach -
1) It cannot be extended distally because of the trifurcation vessels that traverse the interosseous membrane approximately 5 cm below the joint line. However, because the lateral tibial metaphysis has a posterior inclination angle of approximately 45 degree and the posterolateral split fracture segment is usually less than 4 cm in cortical length, this limitation seems to have no problem in practice.
2) Difficult to address additional medial plateau fractures when the patient is lying in the lateral position.
3) Iatrogenic injuries of blood vessels can occur if the posterolateral plate is placed too far distally.
4) Precise knowledge of the anatomy of the posterolateral corner is required.