Kindly listen to this podcast for better understanding https://open.spotify.com/episode/1hZtTtCpyI00m9B29XAEbo
Important ORTHOPEDIC Topics
Monday, May 12, 2025
Thursday, May 1, 2025
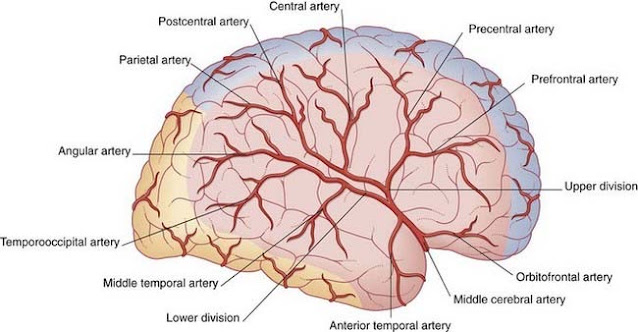
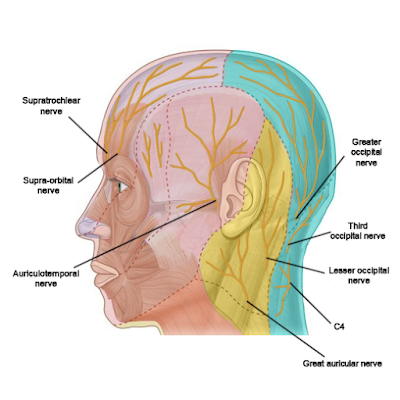
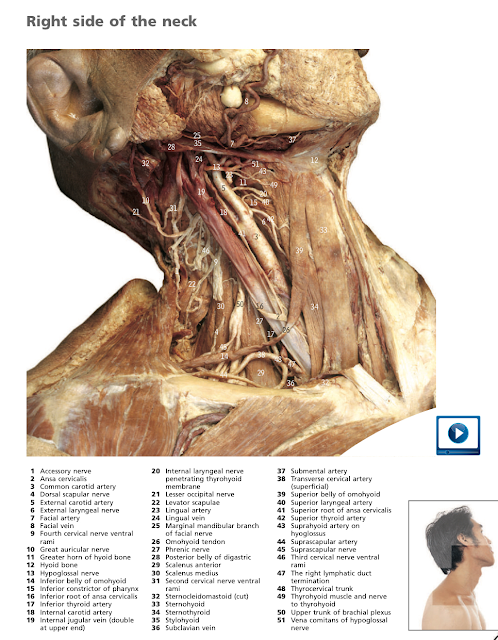
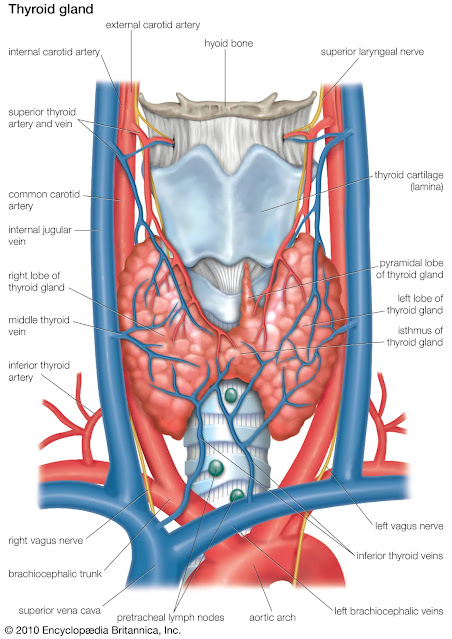
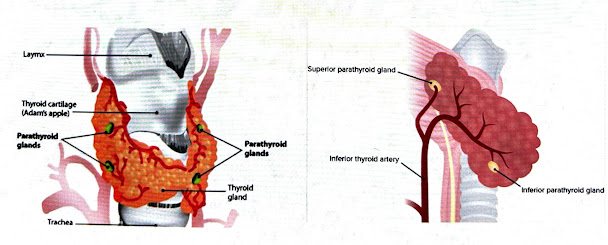
ANATOMY - HEAD & NECK 2 Images
Listen to this Anatomy podcast and revise your Head & Neck topics with images in a timely manner.
https://open.spotify.com/episode/4Ynhn7NdMaJN9VtdRRStIL
Saturday, January 25, 2025
Terrible Triad of Elbow
Introduction -
Originally described in 1996 by Hotchkiss, the terrible triad of the elbow constitutes a highly unstable form of fracture-dislocation consisting of elbow dislocation with concomitant radial head or neck and coronoid process fractures.
Relevant Anatomy
◎ Radial Head-
○ Resists posterolateral rotatory instability
○ Resists Valgus strain to the elbow
◎ Coronoid-
○ Forms the buttress for the ulno-humeral joint
○ Prevents posterior subluxation with elbow from full flexion to 30 degree
◎ Medial collateral ligament
* Anterior bundle
- most important for stability,
- restraint to valgus and posteromedial rotatory instability
- insertion on sublime tubercle (anteromedial facet of coronoid)
* Posterior bundle
* Transverse ligament
◎ Lateral collateral ligament
- Insertion on supinator crest distal to lesser sigmoid notch
- the primary restraint to posterolateral rotatory instability
- Avulsion from lateral condyle when injured
- Components
Lateral ulnar collateral ligament (most important for stability)
Radial collateral ligament
Annular ligament
Accessory ligament
Mechanism and Presentation
◎ Fall on outstretched hand that is in mild flexion
◎ Valgus stress at elbow
◎ Forearm supination
* Evaluation in ED -
○ X-rays
○ NV status
○ Elbow reduction in ED
○ Appropriate immobilisation in above elbow back slab
○ Confirm NV status again
○ Repeat X-rays
○ Check for distal radio-ulnar joint injury (Essex Lopresti injury)
○ CT scan thereafter (can happen from the ward/ED)
Radiographs and definition
◎ Damage/Fracture to radial head 
◎ Damage/Fracture to coronoid
◎ Elbow dislocation
◎ Get pre and post reduction x-rays
◎ Forearm and wrist x-rays - if distal radioulnar joint injury is suspected
Typical images of a reduced elbow with Terrible Triad injury -
Treatment (conservative)
• Indication -
- Ulno-humeral and radio-capitellar joints well reduced
- Radial head # must not meet surgical indications
- Small coronoid (mayo type 1) #
- elbow should be sufficiently stable to allow early ROM
• 1 week of immobilization (at 90 degree)
• Active assisted motion initiated with the splint on.
• ROM from full flexion to progressive extension. Full extension is done around 6-week time.
• Strengthening after 6 weeks
Radial Head Surgical indications
Mason classification
◎ Mason Type II with mechanical block
◎ Mason Type III where ORIF feasible
◎ Presence of other complex ipsilateral elbow injuries
Coronoid fracture
◎ Transverse fractures (Mayo type I)
◎ Anteromedial facet fractures (Mayo type II)
◎ Basilar fractures (Mayo type III)
Management (Surgical)
◎ Indication - Terrible triad injury with
- unstable radial head fracture (meeting surgical indications)
- type II/III coronoid fracture
- Posterior skin incision advantageous
- Radial head-
○ Radial head arthroplasty/excision in severely comminuted # radial head
- Coronoid-
○ FCU split approach for isolated coronoid #
○ Mayo type 1- suture anchor/suture tunnel in unstable elbow
○ Mayo type 2- suture / buttress plate in larger fragment
○ Mayo type 3- Lag screw +/- buttress plate
- LCL repair
○ reattach with suture anchors or trans-osseous sutures
○ if MCL is intact, LCL is repaired with forearm in pronation
○ if MCL injured, LCL is repaired with forearm in supination to avoid medial gapping
○ repairs are performed with elbow at 90 degrees of flexion
- MCL repair
○ Indicated if instability on examination after LCL and fracture fixation, Especially with extension beyond 30 degrees
○ Persistent posteromedial instability following radial head replacement/repair and LCL repair in the setting of Type I/II coronoid fracture should be managed with MCL repair
- Hinged fixators- when instability is noted after complete bone and soft tissue repair
Post Operative
• Immobilize in flexion with forearm pronation to provide stability against posterior
subluxation
• If both MCL and LCL were repaired, elbow in flexion and forearm neutral rotation
• Active ROM exercises 48 hours after surgery
Complications
• Instability- more common following type I or II coronoid fractures
• Failure of internal fixation- more common following repair of radial neck fractures
- poor vascularity leading to osteonecrosis and non-union
• Post-traumatic stiffness
• Heterotopic ossification
- prophylaxis in pts with head injury or in setting of revision surgery
• Post-traumatic arthritis
References -
- Ring D, Jupiter JB, Zilberfarb J. "Terrible Triad Injuries of the Elbow." *J Orthop Trauma.* 2024.
- O’Driscoll SW. "Posterolateral Rotatory Instability of the Elbow." *J Hand Surg.* 2023.
Thank You
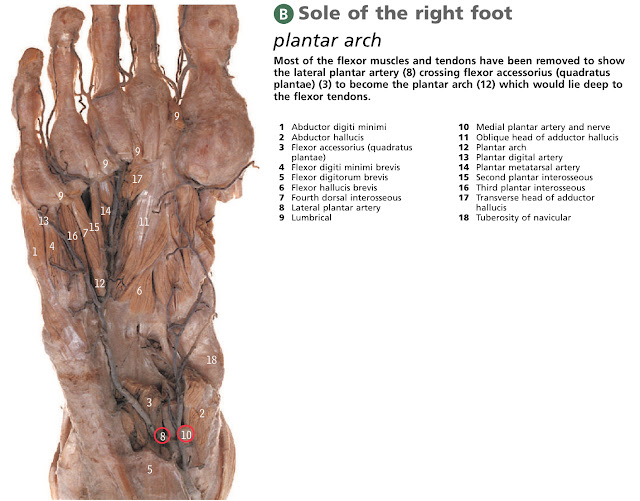
Anatomy - Lower Limb 1
Kindly listen to this podcast for better understanding https://open.spotify.com/episode/1hZtTtCpyI00m9B29XAEbo

-
INTRODUCTION- Views of scaphoid --> X - rotational (pronation/supination); Y -sagittal (flexion/extension); Z - corona...
-
The term 'Remplissage' means 'to fill in'. • 1st described in 2007 by Wolf et al (1) as an adjunct to the arthr...
-
1) DORSAL APPROACH - ☆ Scaphoid Open Reduction and Internal Fixation from the Dorsal Approach/Mini-Open Approach •The ...